About

RaDAR memory clinics are currently provided by primary health care teams in the Saskatchewan communities of Kipling, Bengough, Weyburn, Carlyle, Maryfield, Lampman, Esterhazy, Canora, and Assiniboia. The memory clinics continue to spread in the province, with plans to become available in more communities.
The memory clinics were established to address the need for specialized dementia care in rural communities without travel to a major city.
“It’s a “one-stop-shop”. They come, they do everything at once, and it’s beneficial for families, for clients, that they don’t have to come back again. They get a diagnosis, peace of mind for the family that they get a diagnosis at the end – that what they’re seeing isn’t ‘crazy’. And making a difference in a small town setting.” (Memory Clinic professional)
Patients & Families

“It was a positive experience, from the start through to the finish. And the lead physician was so respectful of my dad….And everyone was just so professional and so patient with him. And always seeking his understanding at all of the juncture points too. So again, leading to a very positive experience.” (Care Partner)
(Care Partner)

- The appointment requires approximately 3 hours.
- Patient and family meet with their memory clinic team to discuss the plan for the appointment.
- Patient and family meets separately with individual team members, with the patient undergoing an assessment with each professional.
- At the end of appointment, the team reviews the assessment findings with patient and family, makes recommendations for management, and plans for follow-up.
- Reduces travel to city-based specialists
- Opportunities to have your questions answered
- Improves understanding of symptoms causing concern
- Provides options for treatment and management
- Connects to available services and support
- Helps plan for the future

- Memory clinics are currently offered by primary health care teams in the Saskatchewan communities of Kipling, Bengough, Weyburn, Carlyle, Maryfield, Lampman, Esterhazy, Canora, and Assiniboia.
- The office staff with each clinic will arrange for a family member or close friend to take part in the appointment, and send a confirmation letter including necessary test requisitions to the patient.
Health Professionals

“…it’s not like reinventing the wheel and starting from scratch. It’s all laid out for you how you set it up and how you do it, so that makes it easier to start a clinic in a town with the support that you get... So, that makes it maybe not quite so daunting of a task.” (Memory Clinic professional)
“We’re working together and pulling depts together for the better of the patient, which is primary health care. We’re wrapping the services around the patient, bringing our therapies, our NP, our physician, Alzheimer Society, kind of that one-stop shop, which is how we’re trying to really build our networks.” (Memory Clinic professional)

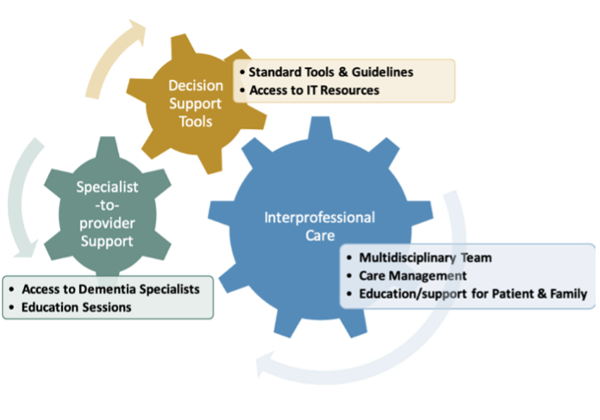
- Memory clinics are adapted to local primary health care teams. Teams include a lead clinician (either a physician or nurse practitioner), home care nurse or social worker, occupational therapist and/or physiotherapist, and Alzheimer Society First Link Coordinator.
- Care management and support for patients and families are provided by home care or social work, and a First Link Coordinator.

- Electronic medical record flow sheets to guide assessments and decision-making include separate sections for each team member. The flow sheets follow the PC-DATA algorithm (Primary Care Dementia Assessment and Treatment Algorithm) based on Canadian guidelines.
- A comprehensive handbook consists of office forms, the PC-DATA education manual, and other resources developed in collaboration with memory clinic teams.
- New teams take part in PC-DATA training with geriatric psychiatrist Dr. Dallas Seitz (University of Calgary) and orientation sessions with the RaDAR team.
- Clinical mentorship and operational guidance for new teams are provided by the lead clinician of the Kipling memory clinic (Jean Daku), Memory Clinic Coordinator (Chelsie Cameron), and the RaDAR team.
- Opportunities are available to new teams to shadow memory clinics in rural communities and the specialist clinic in Saskatoon.
- RaDAR offers interactive education webinars 3-4 times/year to all memory clinic teams, on topics suggested by the teams. Past webinars have covered substance-induced cognitive impairment, management of behavioural symptoms of dementia, legal capacity, dementia and driving, dementia medications, and differential diagnosis.


Locations

Memory clinics are offered by primary health care teams in the Saskatchewan communities of Kipling, Bengough, Weyburn, Carlyle, Maryfield, Lampman, Esterhazy, Canora, and Assiniboia. Download the clinic brochure.
Clinics are held every 1-2 months in each community, and are a part of primary health care team operations within the Saskatchewan Health Authority.
| Bengough: 306-268-2222 | Carlyle: 306-453-6795 |
| Kipling: 306-736-2559 | Weyburn: 306-842-8790 |
| Radville: 306-869-3111 | Maryfield: 306-646-2133 |
| Lampman: 306-487-2811 | Esterhazy: 306-745-6681 |
| Canora: 306-563-5557 | Assiniboia: 306-642-4454 |
A clinic visit with the Kipling Team - a nurse practitioner led team.






A clinic visit with the Esterhazy Team - a family physician led team

2024 Members of the Canora Clinic team (Est. 2024)

Research

The Dementia Working Group guides the research, shares information across health sectors about services and programs, and supports the partnership between RaDAR, the Alzheimer Society, and the memory clinic teams within the Saskatchewan Health Authority.
Objective
To examine the experiences of patients and families receiving memory clinic care, including how they perceive the team-based format of the clinics and how care can be further improved
Methods
- Mail-in questionnaire and short telephone interviews with patients and families attending RaDAR memory clinics
Preliminary Findings (2021 RaDAR Primary Care Memory Clinics Update)
- As Covid-19-related disruptions to the memory clinics decrease, we will continue to collect patient and family experiences of assessment and diagnosis at the clinics. Feedback continues to be very positive, especially regarding the primary health care team members and how they collaborate to provide a supportive environment for assessment, diagnosis, and future planning. Patients and families are happy with the Covid-19 protocols put in place and still feel satisfied about their clinic experiences with assessment and diagnosis. As the rural memory clinics spread to additional areas of Saskatchewan and new PHC teams, ongoing process feedback from patients and their families will help to ensure the memory clinics are functioning well and whether there are areas for further improvement.
Objective
To qualitatively explore memory clinic patients’ quality of life and factors associated with quality of life, as well as health and community service usage and unmet needs
Methods
- Semi-structured telephone interviews with memory clinic patients take place shortly after clinic day and three months later.
Objective
To examine reasons for referral to RaDAR memory clinics, patient characteristics, and recommendations and referrals after initial memory clinic evaluation
Methods
- Retrospective analysis of selected PC-DATA and other information collected for patients seen in memory clinics from Dec 1/17 to Nov 30/21.
Objective
To examine the role and impact of including a First Link Coordinator in RaDAR memory clinics
Methods
- Semi-structured telephone interviews with 3 First Link Coordinators serving 4 RaDAR memory clinic teams
- Alzheimer Society of Saskatchewan e-Tapestry database data comparing RaDAR Memory Clinic, self, and direct referrals from primary care professional
Poster
Morgan, D., Bayly, M., Kosteniuk, J. Perceptions and outcomes of an embedded Alzheimer Society First Link Coordinator in rural primary healthcare memory clinics. A poster presentation at the Canadian Association on Gerontology Conference, Regina, October 20-22, 2022.
To conduct an evaluation of the Kipling Active Living Program during the initial stages of the 8-wk program to determine whether short-term outcomes are meeting expectations
Methods
- Self-report questionnaire completed by 5 participants
- Participant well-being assessment completed by 7 participants on the first day of the 8-wk program (pre) and 5 participants on the last day (post)
Preliminary findings
- The initial goals of cognitive, social, and physical stimulation were addressed. Participants reported highly positive experiences in terms of the varied and engaging program activities, opportunities for visiting, and interactions with program staff. The program appears to fill a gap for people with cognitive impairment and dementia living in Kipling and surrounding areas.
Objective
To identify and describe programs and services for older adults in RaDAR memory clinic communities and surrounding areas
Methods
- Focus group with health care professionals and managers; review of secondary sources of information; systematic internet search
- Interviews with caregivers of older adults living with dementia in these rural areas
What we've learned so far:
A range of available services (43) were identified, categorized into 7 service types, and mapped by location. Most services were Social/Leisure Activities (n=14), then General Support/Referrals (n=13), Transportation (n=7), Information/Education (n=4), Respite (n=2), Home/Personal Care (n=2), and Safety (n=1). Most involved no fees, referral by self/other, and a range of provider education/training. Twenty services across 4/7 types were offered remotely. In-person dementia-specific services were lacking. Caregiver interviews (5) have been completed and analyses is underway. Findings may inform future service delivery, interventions, and improve local program participation.
Poster
Elliot V., Morgan D., Kosteniuk J., Bayly M., Cameron C., O'Connell M.E. Environmental scann of community-based programs for older adults in rural memory clinic communities and surrounding areas. A poster presentation at the 35th Global Conference of Alzheimer’s Disease International (virtual format), June 9-11, 2022.
Objective
To examine service/support use and experiences among family care partners participating in an initial RaDAR memory clinic assessment of their family member
Methods
- First semi-structured interview in-person with carer at initial memory clinic evaluation and collection of patient information (age, sex, cognitive and functional scores)
- Second interview with carer by telephone 1 month after initial memory clinic evaluation
Poster
Kosteniuk J., Morgan D., O’Connell M., Cameron C., Elliot V., Bayly M. Service use and self-efficacy of family carers participating in a rural primary health care memory assessment. A poster presentation at the 35th Global Conference of Alzheimer’s Disease International (virtual format), June 9-11, 2022.
Publications

Morgan et al. 2022. Factors influencing sustainability and scale-up of rural primary healthcare memory clinics: Perspectives of clinic team members. BMC Health Services Research, 22, 148. doi:10.1186/s12913-022-07550-0
Morgan et al. 2019. Barriers and Facilitators to Development and Implementation of a Rural Primary Health Care Intervention for Dementia: A Process Evaluation. BMC Health Services Research, 19:709. doi:10.1186/s12913-019-4548-5
Morgan et al. 2019. A 5-step approach for developing and implementing a rural primary health care model for dementia: A community-academic partnership. Primary Health Care Research & Development, 20 (e29). doi:10.1017/S1463423618000968
Kosteniuk et al. 2022. Dementia-related continuing education for rural interprofessional primary health care: perceptions and needs of webinar participants. Primary Health Care Research and Development, 23 (e32): 1–7. doi.org/10.1017/S1463423622000226
2024 Update: RaDAR Primary Care Memory Clinics (7 MB). Saskatoon, Saskatchewan: University of Saskatchewan, 14 Pages.
2023 Update: RaDAR Primary Care Memory Clinics (1.5 MB). Saskatoon, Saskatchewan: University of Saskatchewan, 13 Pages.
2022 Update: RaDAR Primary Care Memory Clinics (1 MB). Saskatoon, Saskatchewan: University of Saskatchewan.
2021 Update: Rural Memory Clinics (1 MB). Saskatoon, Saskatchewan: University of Saskatchewan.
Rural PHC Memory Clinics: 2020 Report (0.5 MB). Saskatoon, Saskatchewan: University of Saskatchewan.
Rural PHC Memory Clinics: Fall 2019 (4 MB). Saskatoon, Saskatchewan: University of Saskatchewan.
Media

Podcast introduction to the Kipling Memory Clinic, featuring the story of Leanne and her mother Marjory, supported by Jean Daku, Kipling Nurse Practitioner. Dementia Dialogue System Journey Podcast Series. Transitions- A Rural Dementia Resource for rural communities. Sept 28, 2020.
Analysis & Policy Observatory Guest blog by Dr. Debra Morgan, RaDAR Lead. Rural Dementia in Action by Debra Morgan. August 16, 2020.
Reflection article by Jennifer Hill, Primary Health Care Facilitator with the Weyburn Memory Clinic Team. Embracing Research in Rural Dementia Care. December 18, 2019.
Story about Rural PHC Memory Clinics in SaskHealth (page 13), Saskatchewan Health Authority's annual report to the community. Dementia care program provides care closer to home (15 MB). December 2, 2019.
Interview of Dr. Debra Morgan by Drew Wilson, CJWW Radio. Bringing Dementia Care into Rural Saskatchewan. September 19, 2019.
Backgrounder on Rural PHC Memory Clinic model on Saskatchewan Health Authority website. RaDAR – The Rural Dementia Action Research Team. September 12, 2019.
SHRF support of Rural PHC Memory Clinics on Saskatchewan Health Research Foundation website. Building Capacity for Rural and Remote Dementia Care. September 12, 2019.
Profile of Rural PHC Memory Clinics on Saskatchewan Health Authority website. RaDAR: Dementia care close to home. August 8, 2019.
Contact

For more information about the clinics:
- Contact a clinic
- Call or email research program lead: Dr. Debra Morgan at 306-966-7905 or debra.morgan@usask.ca
Background & Funding
For more than 20 years, RaDAR lead Dr. Debra Morgan has been researching and applying ways to improve the quality of life for people living with dementia in rural and remote communities.
The memory clinics were informed by the RRMC, a specialist clinic located at the University of Saskatchewan in Saskatoon. The RRMC offers a full-day interdisciplinary assessment to people living with suspected atypical and complex dementia across rural and remote Saskatchewan.
Research funding is provided by a Canadian Institutes of Health Research Foundation grant to Dr. Morgan, and funding from the Saskatchewan Health Research Foundation through Phase 2 of the Canadian Consortium on Neurodegeneration in Aging (Team 15 Co-Leads Drs. Megan O’Connell and Debra Morgan).


